Nh Magellan Medicaid Prior Template
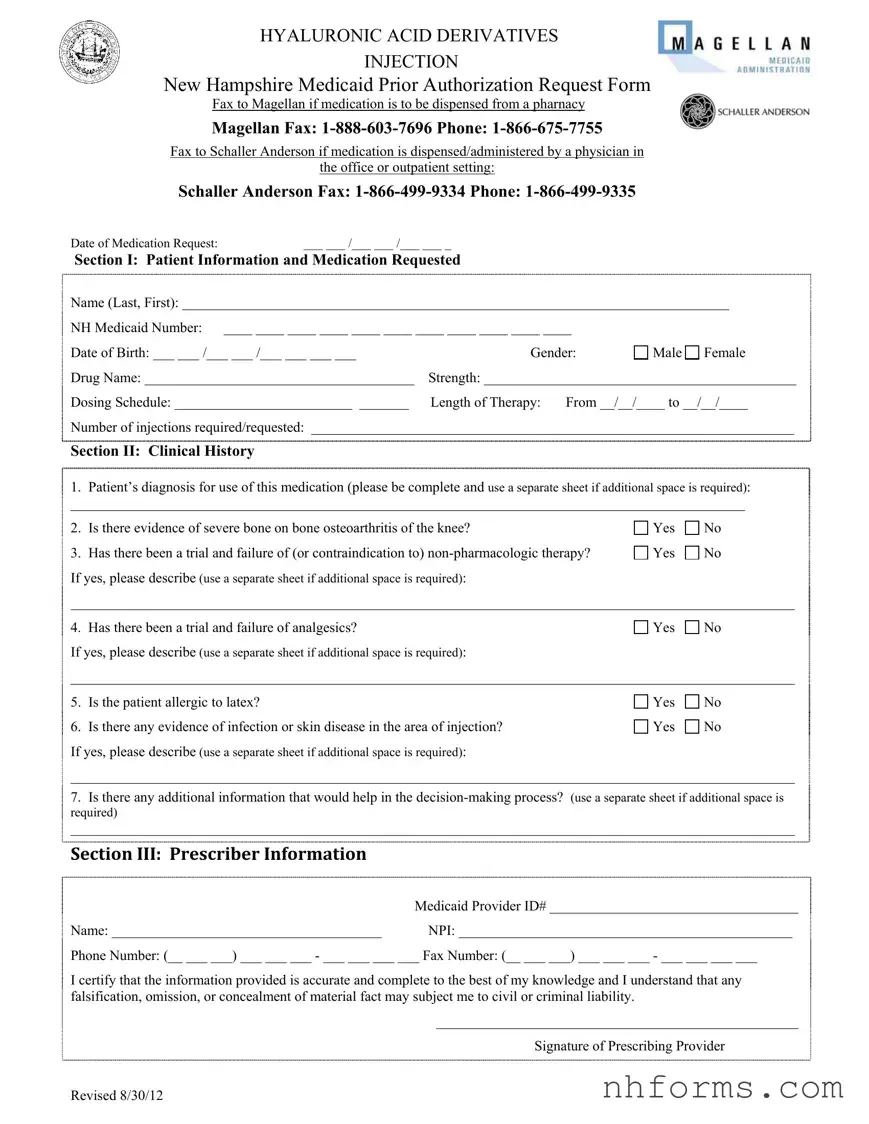
Navigating the intricacies of healthcare forms can often feel daunting, yet understanding them is crucial for the provision of timely medical care. The NH Magellan Medicaid Prior Authorization Request Form serves as a key document within this process, specifically for patients in New Hampshire needing hyaluronic acid derivative injections. This form must be submitted to Magellan for medications dispensed from a pharmacy or to Schaller Anderson for medications administered by a physician in an office or outpatient setting—a distinction that underscores the form's dual pathway depending on the treatment's administration location. It meticulously collects patient information, including Medicaid number and medication specifics like drug name, strength, and dosing schedule, alongside a section dedicated to the required clinical history. The form delves into the patient's diagnosis, previous treatments, and any contraindications, ensuring a comprehensive review to support the authorization request. Prescriber details are also captured, with a certification that the information provided is both accurate and complete, highlighting the form's role in facilitating communication between healthcare providers and payers to secure necessary patient treatments. Revised on August 30, 2012, this document underscores the complexities of managed care under Medicaid, reflecting the broader challenges of navigating the healthcare system's administrative demands.
Document Preview Example
HYALURONIC ACID DERIVATIVES
INJECTION
New Hampshire Medicaid Prior Authorization Request Form
Fax to Magellan if medication is to be dispensed from a pharnacy
Magellan Fax:
Fax to Schaller Anderson if medication is dispensed/administered by a physician in
the office or outpatient setting:
Schaller Anderson Fax:
Date of Medication Request: |
___ ___ /___ ___ /___ ___ _ |
|
|
|
Section I: Patient Information and Medication Requested |
|
|
||
Name (Last, First): _____________________________________________________________________________ |
||||
NH Medicaid Number: |
____ ____ ____ ____ ____ ____ ____ ____ ____ ____ ____ |
|
||
Date of Birth: ___ ___ /___ ___ /___ ___ ___ ___ |
Gender: |
Male Female |
||
Drug Name: ______________________________________ |
Strength: ____________________________________________ |
|||
Dosing Schedule: _________________________ ________ |
Length of Therapy: |
From __/__/____ to __/__/____ |
||
Number of injections required/requested: ____________________________________________________________________
Section II: Clinical History
1.Patient’s diagnosis for use of this medication (please be complete and use a separate sheet if additional space is required):
_______________________________________________________________________________________________
2. |
Is there evidence of severe bone on bone osteoarthritis of the knee? |
Yes |
No |
3. |
Has there been a trial and failure of (or contraindication to) |
Yes |
No |
If yes, please describe (use a separate sheet if additional space is required): |
|
|
|
______________________________________________________________________________________________________
4. Has there been a trial and failure of analgesics? |
Yes |
No |
If yes, please describe (use a separate sheet if additional space is required): |
|
|
______________________________________________________________________________________________________
5. |
Is the patient allergic to latex? |
Yes |
No |
6. |
Is there any evidence of infection or skin disease in the area of injection? |
Yes |
No |
If yes, please describe (use a separate sheet if additional space is required):
______________________________________________________________________________________________________
7.Is there any additional information that would help in the
______________________________________________________________________________________________________
SECTION III: PRESCRIBER INFORMATION
|
Medicaid Provider ID# ___________________________________ |
Name: ______________________________________ |
NPI: _______________________________________________ |
Phone Number: (__ ___ ___) ___ ___ ___ - ___ ___ ___ ___ Fax Number: (__ ___ ___) ___ ___ ___ - ___ ___ ___ ___
I certify that the information provided is accurate and complete to the best of my knowledge and I understand that any falsification, omission, or concealment of material fact may subject me to civil or criminal liability.
___________________________________________________
Signature of Prescribing Provider
Revised 8/30/12
Document Breakdown
| Fact | Detail |
|---|---|
| Purpose | Request prior authorization for hyaluronic acid derivatives injection for New Hampshire Medicaid recipients |
| Submission Process | Forms must be faxed to Magellan for medications dispensed from a pharmacy or to Schaller Anderson if medication is administered by a physician in an office or outpatient setting |
| Magellan Contact Information | Fax: 1-888-603-7696, Phone: 1-866-675-7755 |
| Schaller Anderson Contact Information | Fax: 1-866-499-9334, Phone: 1-866-499-9335 |
| Sections | The form is divided into three sections: Patient Information and Medication Requested, Clinical History, and Prescriber Information |
| Key Criteria for Approval | Evidence of severe bone on bone osteoarthritis of the knee, trial and failure of non-pharmacologic therapy and analgesics, absence of latex allergy, and no infection or skin disease in the area of injection |
| Specific Instructions | Comprehensive information including diagnosis, clinical history, and additional relevant information is required. Use of separate sheets for additional space is allowed |
| Governing Law(s) | The form adheres to New Hampshire Medicaid regulations and requirements for prior authorization of specific medical treatments |
Detailed Instructions for Writing Nh Magellan Medicaid Prior
Completing the New Hampshire Medicaid Prior Authorization Request Form for hyaluronic acid derivatives injection is a critical step in ensuring that patients receive necessary medical treatments in a timely manner. This form is vital for healthcare providers who are seeking approval from Medicaid before administering specific medications. The process involves detailed documentation about the patient's medical need for the medication, including diagnosis and previous treatments. Filling out this form accurately is essential for a smooth approval process. Below is a guide to assist you in completing each section of the form.
- Date of Medication Request: Indicate the date when the request is being made by filling in the date in the format mm/dd/yyyy.
- Section I: Patient Information and Medication Requested
- Fill in the patient's name, starting with the last name followed by the first name.
- Enter the NH Medicaid Number of the patient as a continuous string of digits without spaces.
- Provide the patient's date of birth in the format mm/dd/yyyy.
- Indicate the patient’s gender by checking the appropriate option.
- Write down the name of the drug and its strength.
- Specify the dosing schedule.
- State the length of therapy, indicating the start and end dates.
- Enter the number of injections required or requested.
- Section II: Clinical History
- Provide a comprehensive diagnosis that justifies the use of the medication.
- Answer whether there is evidence of severe bone on bone osteoarthritis of the knee.
- Indicate if there has been a trial and failure of (or contraindication to) non-pharmacologic therapy.
- Document any trial and failure of analgesics.
- Answer if the patient is allergic to latex.
- State if there is any evidence of infection or skin disease in the area of injection.
- Provide any additional information that would assist in the decision-making process.
- Section III: Prescriber Information
- Enter the Medicaid Provider ID number.
- Fill in the name of the prescribing provider.
- Provide the National Provider Identifier (NPI) number.
- Include the phone and fax numbers with the area code.
- Lastly, the prescriber must sign the form to certify that all the information provided is accurate and complete. Ensure the signature and date are clear.
After completing the form, it's essential to send it to the correct fax number based on the medication's dispensing location. If the medication will be dispensed from a pharmacy, fax the form to Magellan using the provided fax number. In cases where the medication is administered by a physician in an office or outpatient setting, the form should be faxed to Schaller Anderson. This distinction is crucial for proper routing and timely processing of the request. Following these steps accurately will aid in the smooth processing of the prior authorization request, ultimately benefiting the patient’s access to necessary medication.
Essential Queries on Nh Magellan Medicaid Prior
What is the NH Magellan Medicaid Prior Authorization Request Form used for?
The NH Magellan Medicaid Prior Authorization Request Form is specifically designed for requesting authorization for Hyaluronic Acid Derivatives Injection for New Hampshire Medicaid patients. This form is essential when these medications need to be dispensed from a pharmacy or administered by a physician in an office or outpatient setting. It helps ensure that the medication is covered under the patient's Medicaid plan before it is provided, ensuring both compliance and coverage for necessary treatments.
Who needs to fill out this form?
The prescribing provider, who has evaluated the patient's medical condition and determined the need for Hyaluronic Acid Derivatives Injection, is required to fill out this form. It's crucial that the provider includes detailed patient information, clinical history relating to the medication request, and their professional details for contact and verification purposes.
Where should the form be faxed depending on the medication dispensation method?
If the medication is to be dispensed from a pharmacy, the form should be faxed to Magellan at 1-888-603-7696. However, if the medication is dispensed or administered by a physician in the office or an outpatient setting, the form should be faxed to Schaller Anderson at 1-866-499-9334. This ensures the request is directed to the appropriate channel for processing.
What information is required in the Clinical History section?
In the Clinical History section, detailed information regarding the patient's diagnosis for which the Hyaluronic Acid Derivatives Injection is being requested must be provided. This includes evidence of severe bone on bone osteoarthritis of the knee, any trials and failures of non-pharmacologic therapy or analgesics, latex allergies, or the presence of any infection or skin disease in the area of injection. These details are crucial for understanding the necessity of the treatment and its urgency.
Is there a requirement for providing additional information?
Yes, if the prescribing provider believes there is additional information that could aid in the decision-making process regarding the authorization request, they are encouraged to include this on a separate sheet. This could encompass any relevant medical history or other factors that justify the need for the medication.
What is the significance of the prescribing provider's certification on the form?
By signing the form, the prescribing provider certifies that the information provided is accurate and complete to the best of their knowledge. This is a declaration of the truthfulness and reliability of the information submitted. It's a crucial step as falsification, omission, or concealment of material fact may subject the provider to civil or criminal liability. It emphasizes the seriousness of the authorization process.
How does one know if the medication is approved?
Once the form has been submitted, it will be reviewed by the appropriate authority (Magellan or Schaller Anderson, depending on where the medication is dispensed from). The prescribing provider will then be notified of the approval or denial of the authorization request. It is vital for providers to provide accurate and reachable contact information for efficient communication.
Can the form be submitted for multiple injections?
Yes, the form allows the prescribing provider to request a specific number of injections as required for the patient's treatment plan. The "Number of injections required/requested" section on the form should be utilized to specify this information clearly, aligning the treatment with the patient's health needs.
What happens if there's an error on the form?
If an error is discovered on the form after submission, it's important for the prescribing provider to contact Magellan or Schaller Anderson immediately, depending on where the form was initially submitted. Corrections or amendments might require refilling and resubmitting the form with the accurate information to ensure proper processing of the authorization request.
Where can one find more information or assistance with the form?
For additional assistance or questions regarding the NH Magellan Medicaid Prior Authorization Request Form, prescribing providers can contact Magellan at 1-866-675-7755 or Schaller Anderson at 1-866-499-9335, depending on the dispensation method of the medication. These contacts can provide guidance, answer questions, and offer support throughout the authorization process.
Common mistakes
Filling out the NH Magellan Medicaid Prior Authorization Request Form is a critical step in the process of obtaining certain medications under New Hampshire Medicaid. However, it's common for individuals to make mistakes when completing this form, which can delay the approval process or lead to denial of the medication requested. Here are ten mistakes to avoid:
- Not providing complete patient information in Section I, including the full name, NH Medicaid Number, and date of birth. These details are essential for identifying the patient within the Medicaid system.
- Incorrectly filling out the date of medication request. It's important to use the MM/DD/YYYY format to avoid confusion and ensure the form is processed in a timely manner.
- Omitting the drug name and strength in the medication requested section. This information is crucial for the pharmacy or physician to know what specific medication and dose are being authorized.
- Failing to specify the dosing schedule and length of therapy. These details help the reviewing authority understand the planned treatment duration and frequency of the injections required.
- Not accurately detailing the patient’s clinical history in Section II. The decision to authorize the medication often hinges on this information, including diagnosis, previous treatments, and any contraindications.
- Leaving the sections about trials of non-pharmacologic therapy and analgesics blank or inadequately explained. Evidence of trying and failing other treatments is usually required before authorization for certain medications.
- Forgetting to indicate whether the patient is allergic to latex, which is vital considering the potential for allergic reactions during medication administration.
- Neglecting to describe any evidence of infection or skin disease in the area of injection. This information is crucial for assessing the suitability of the injection treatment.
- Omitting additional information that might help in the decision-making process. Sometimes, providing extra details can make a significant difference in getting authorization for the medication.
- In Section III, failing to include accurate prescriber information, such as the Medicaid Provider ID, NPI, and contact details. Additionally, ensuring the prescriber's signature is on the form certifies the accuracy and completeness of the information provided.
Avoiding these mistakes can significantly impact the approval process. Taking the time to double-check and ensure all the required information is provided accurately and completely can help smooth the path for getting necessary medications approved under New Hampshire Medicaid. Engaging with healthcare providers for assistance and clarification when in doubt can also be incredibly beneficial. Remember, the goal of the prior authorization process is to ensure that patients receive the most appropriate and cost-effective treatments available under their insurance plans, and accurately completing this form is a key step in that process.
Documents used along the form
When dealing with the complex world of medical documentation and prior authorizations, especially in the realm of Medicaid, understanding the right forms to use—and when—is crucial. The New Hampshire Magellan Medicaid Prior Authorization form for hyaluronic acid derivatives injection is a key document in managing care for patients who require specific treatments. However, this form doesn't stand alone. Several other documents often accompany it or are necessary for a seamless process, ensuring comprehensive care and compliance with medical and legal standards.
- Medical Records Release Form: This form is essential for sharing patient medical records between healthcare providers. It ensures that a patient's health information is securely transferred and that there's comprehensive data to support the medical necessity of the treatment requested.
- Patient Consent Form: Before any treatment is administered, especially involving medications or procedures requiring prior authorization, a patient must provide informed consent. This document outlines the risks, benefits, and alternatives to the proposed treatment.
- Insurance Verification Form: This document is vital for confirming the patient’s coverage specifics, including eligibility dates, covered benefits, and patient responsibility for co-pays or deductibles. It aids in ensuring that treatments are covered before they are administered.
- Treatment Plan Form: A detailed outline of the proposed treatment, including the rationale for selecting specific medications or therapies, goals of treatment, and expected outcomes. This form provides a roadmap for care and is crucial for obtaining prior authorization.
- Prescription Form: While a part of the prior authorization process involves detailing the medication requested, a separate prescription form, completed by the healthcare provider, might also be necessary, especially for pharmacy-dispensed medications.
- Appeal Form: If a treatment or medication request is denied, an appeal form becomes necessary. This document is used to contest a decision, providing additional information or clarification to support the medical necessity of the requested service.
- Denial Letter: Should an authorization request be denied, a denial letter from the insurance or Medicaid will detail the reasons for denial and provide information on how the decision can be appealed.
- Referral Form: In cases where a specialist's evaluation or treatment is necessary, a referral form from the primary care provider is often required. This form indicates the need for specialized services and supports the request for specific treatments.
Navigating healthcare procedures requires a keen understanding of documentation and regulatory requirements. For patients, their families, and healthcare providers working within the Medicaid system, these forms represent steps towards receiving the necessary and appropriate medical care. The importance of filling out these documents accurately and completely cannot be overstated, both for legal compliance and for the well-being of the patient.
Similar forms
The NH Magellan Medicaid Prior Authorization Request Form is similar to various other healthcare documentation forms required for the processing of medication prescriptions within different healthcare systems. These documents broadly serve to ensure that prescribed medications are covered by a patient's healthcare plan, confirm medical necessity, and facilitate proper medication management.
One example of a similar document is the Medicare Part D Coverage Determination Request Form. Just like the NH Magellan Medicaid Prior Authorization Request form, this document is used by healthcare providers to request approval for a prescription drug under the Medicare Part D benefit. Both forms require detailed patient information, a section on the medication requested including the drug name, dosage, and length of therapy, and a thorough clinical rationale explaining why the medication is necessary. The key similarity lies in their function to streamline the approval process for medication coverage, ensuring patients receive timely access to necessary treatments.
Another document that shares similarities is the Prior Authorization Request Form used by private insurance companies. Although the format and specific requirements may vary from insurer to insurer, the fundamental purpose aligns closely with the NH Magellan Medicaid Prior form. These forms typically include sections for patient demographics, prescribing provider information, and detailed medication requests coupled with clinical justifications. The essence of both documents is to evaluate the necessity and appropriateness of prescribed medications, thereby managing costs and ensuring the efficacy and safety of treatments provided to patients.
Furthermore, the Exception Request Form found in many healthcare settings, used when a prescribed medication is not on the preferred drug list or formulary, echoes the purpose and structure of the NH Magellan Medicaid Prior Authorization form. Exception Request Forms also gather comprehensive patient and prescriber information, alongside detailed medication requests and clinical justifications, to assess the need for an exception to standard medication policies. This process mirrors the NH Magellan's form's goal of facilitating access to medications that are critical for the patient's health, even if they don't initially meet standard coverage criteria.
Dos and Don'ts
When completing the New Hampshire Magellan Medicaid Prior Authorization Request Form for hyaluronic acid derivatives injection, it's important to approach the task with attention to detail and thoroughness. Below are lists of what you should and shouldn't do to ensure the process goes smoothly and effectively.
Things You Should Do:
- Verify all contact information: Ensure the fax numbers and phone numbers for Magellan and Schaller Anderson are current. This information is crucial for the submission process.
- Fill in all sections completely: Provide complete details in each section, including patient information, clinical history, and prescriber information. Omitting details can delay the process.
- Include the diagnosis with specificity: Clearly state the patient’s diagnosis in Section II, providing enough detail to support the request for medication.
- Document previous treatments: If applicable, describe previous treatments and their outcomes, particularly noting any trials and failures of non-pharmacologic therapy or analgesics.
- Sign and date the form: Make sure the prescribing provider signs and dates the form, certifying that the information is accurate and complete.
Things You Shouldn't Do:
- Leave sections blank: Avoid leaving any sections of the form incomplete. If a section does not apply, indicate this with “N/A” or a similar notation.
- Use unclear handwriting: If filling out the form by hand, write legibly to prevent any misunderstandings or errors in processing the form.
- Forget to include additional sheets if needed: If you run out of space in any section, particularly in documenting the patient’s clinical history, attach additional sheets as necessary.
- Submit without reviewing for accuracy: Double-check all entries for accuracy before submission to avoid delays caused by errors or omissions.
- Ignore deadlines: Keep track of any deadlines associated with the authorization request to ensure the form is submitted in a timely manner.
Misconceptions
There are several common misconceptions about the New Hampshire Magellan Medicaid Prior Authorization Request Form for hyaluronic acid derivatives injections. Addressing these misconceptions can help ensure that individuals are better informed about the process and requirements.
- Misconception #1: The form can be used for any medication. In reality, this specific form is dedicated to requesting prior authorization for hyaluronic acid derivatives injections only.
- Misconception #2: Prior authorization is optional. In fact, obtaining prior authorization through this form is a mandatory step for Medicaid coverage of these injections if they are to be dispensed from a pharmacy or administered by a physician in an office or outpatient setting.
- Misconception #3: One fax number works for all requests. The correct fax number depends on how the medication is dispensed. If it's from a pharmacy, the form should be faxed to Magellan. If administered by a physician, it goes to Schaller Anderson.
- Misconception #4: Only basic patient information is needed. Detailed patient information, including a comprehensive clinical history and the specific diagnosis requiring the use of hyaluronic acid injections, is essential for the form to be processed.
- Misconception #5: Any doctor can request authorization. The request must be made by a Medicaid-enrolled prescriber who signs and certifies that the information provided is accurate to the best of their knowledge.
- Misconception #6: The form doesn't require detailed information about previous treatments. Contrarily, the form requires detailed descriptions of past treatments, including trials and failures of non-pharmacologic therapy and analgesics.
- Misconception #7: The decision for approval is based solely on the form. While the form is critical, the decision-making process may also consider additional information or documentation that supports the necessity and appropriateness of the treatment.
Understanding these aspects of the NH Magellan Medicaid Prior Authorization Request Form can help streamline the process, ensuring that necessary treatments are obtained more efficiently and effectively.
Key takeaways
When handling the New Hampshire Medicaid Prior Authorization Request Form for hyaluronic acid derivatives injections, it is essential to keep several key points in mind to ensure the request is processed smoothly:
- Understand the specific fax numbers: There are two distinct fax numbers provided, each serving a different purpose. If the medication is to be dispensed from a pharmacy, the form should be faxed to Magellan at 1-888-603-7696. Conversely, if the medication is dispensed or administered by a physician in an office or outpatient setting, it should be faxed to Schaller Anderson at 1-866-499-9334. Knowing where to send the form based on the medication dispensation method is crucial for timely processing.
- Complete patient information accurately: Section I of the form requires detailed patient information including the name, New Hampshire Medicaid number, date of birth, gender, and specific medication details such as drug name, strength, dosing schedule, length of therapy, and number of injections needed. Accurately filling out this information is crucial for the processing of the form.
- Provide comprehensive clinical history: The form requires an extensive clinical history in Section II, including diagnosis, evidence of severe bone on bone osteoarthritis of the knee, trials and failures of non-pharmacologic therapy and analgesics, allergies to latex, and any skin infections or diseases in the area of the injection. This detailed information helps in the decision-making process for authorization.
- Include prescriber information and certification: The prescribing provider must furnish their Medicaid Provider ID, name, NPI (National Provider Identifier), phone number, and fax number in Section III. Importantly, the provider must sign the form, certifying that all provided information is accurate and complete to the best of their knowledge. This acts as a safeguard against falsification and ensures accountability.
- Utilize additional space if needed: Throughout the form, there are prompts indicating that additional sheets may be used if required. This is particularly significant for providing a complete patient clinical history or when any section requires more detail than the provided space allows. Utilizing additional sheets helps in offering a thorough explanation or narrative that can support the authorization request.
By closely adhering to these guidelines, healthcare providers can enhance the likelihood of a successful prior authorization for hyaluronic acid derivatives injections under the New Hampshire Medicaid program.
Different PDF Templates
Nh Bugs - Facilitates the required reporting of new employees or independent contractors by New Hampshire businesses, reducing paperwork.
New Hampshire Load - By certifying familiarity with all relevant laws and regulations, applicants demonstrate due diligence in preparing for safe transport.
Nh Criminal Records - Mandates the inclusion of a petitioner's conviction history and the status of their rehabilitation efforts to assess readiness for reintegration into society.