New Hampshire 3820 Template
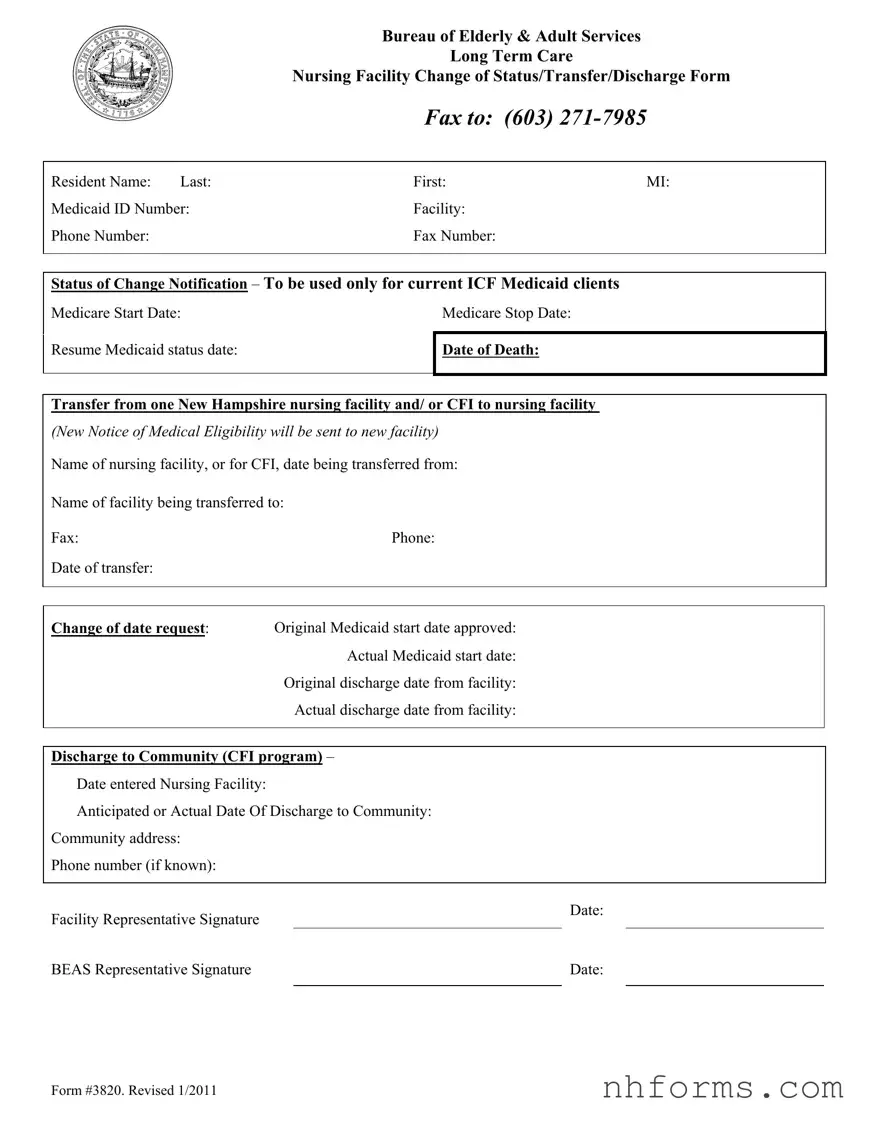
In the intricate landscape of elder care, the New Hampshire 3820 form emerges as a pivotal document for regulating the status changes of individuals residing in long-term nursing facilities. Administered by the Bureau of Elderly & Adult Services, this form serves as a comprehensive notification tool for reporting significant events in a resident's journey, including transfers between facilities, changes in Medicaid and Medicare statuses, and discharges into the community. Its detailed sections demand accurate information about the resident, such as name, Medicaid ID, and the facilities involved in the transfer or discharge process, ensuring that both the sending and receiving institutions, along with the state's administrative bodies, stay well-informed. The form delineates various scenarios, from initiating or ceasing Medicare to resuming Medicaid and even detailing the resident's passage should they decease or transition back into community living. Each segment, meticulously crafted, underscores the importance of timing and precision in the conveyance of changes. The document also requires authentication from representatives of both the facility and the Bureau of Elderly & Adult Services, imbuing it with legal significance and operational gravity. By facilitating a seamless flow of vital data, the New Hampshire 3820 form plays a crucial role in preserving the rights, well-being, and continuity of care for the state's elder and adult residents in nursing facilities.
Document Preview Example
|
Bureau of Elderly & Adult Services |
||
|
|
Long Term Care |
|
|
Nursing Facility Change of Status/Transfer/Discharge Form |
||
|
FAX TO: |
(603) |
|
|
|
|
|
Resident Name: Last: |
First: |
MI: |
|
Medicaid ID Number: |
Facility: |
|
|
Phone Number: |
Fax Number: |
|
|
|
|
||
|
|
||
Status of Change Notification – To be used only for current ICF Medicaid clients |
|||
Medicare Start Date: |
|
Medicare Stop Date: |
|
|
|
|
|
Resume Medicaid status date:
Date of Death:
Transfer from one New Hampshire nursing facility and/ or CFI to nursing facility
(New Notice of Medical Eligibility will be sent to new facility) Name of nursing facility, or for CFI, date being transferred from:
Name of facility being transferred to:
Fax:Phone:
Date of transfer:
Change of date request: Original Medicaid start date approved: Actual Medicaid start date:
Original discharge date from facility:
Actual discharge date from facility:
Discharge to Community (CFI program) –
Date entered Nursing Facility:
Anticipated or Actual Date Of Discharge to Community:
Community address:
Phone number (if known):
Facility Representative Signature
Date:
BEAS Representative Signature |
|
Date: |
|
|
|
Form #3820. Revised 1/2011
Document Breakdown
| Fact | Detail |
|---|---|
| Purpose | The form is designed to notify about a change of status, transfer, or discharge of a resident in a long-term care nursing facility within New Hampshire. |
| Governing Law(s) | This form is governed by New Hampshire state regulations concerning the elderly and adult services, specifically tailored to Medicaid clients in long-term care facilities. |
| Key Information Required | Includes the resident's name, Medicaid ID number, facility details, status of change, and relevant dates (start/stop/resume Medicaid, date of death, transfer, discharge). |
| Usage | Used exclusively for current Medicaid clients in Intermediate Care Facilities (ICFs) within New Hampshire to communicate changes that may affect their state-funded care. |
Detailed Instructions for Writing New Hampshire 3820
Navigating the process of filling out administrative forms can sometimes feel like trying to decipher an ancient code. Today, we're breaking down the steps to fill out the New Hampshire 3820 form, specifically designed for the Bureau of Elderly & Adult Services. This form is essential for reporting changes, including transfers or discharges, regarding long-term care nursing facility residents who are Medicaid clients. Before jumping into the how-to, remember that accurate and prompt completion of this form is crucial. It ensures the resident's care and financial support are not interrupted. Below are the step-by-step instructions to guide you through filling out the form seamlessly.
- Begin by entering the resident's name in the provided fields, including the last name, first name, and middle initial (MI).
- Fill in the Medicaid ID Number to identify the resident within the Medicaid system accurately.
- Provide the name of the facility where the resident is or was located, along with the facility's phone and fax numbers.
- Under the Status of Change Notification section, select the type of change by filling the relevant information, such as:
- For a Medicare coverage change, provide the Medicare Start and Stop Date.
- If resuming Medicaid status, specify the date.
- For a transfer, fill in the names of the origin and destination facilities, including phone and fax numbers, and the date of transfer.
- If there's a change in Medicaid start dates or discharge dates, note the original and actual dates.
- For a discharge to the community, indicate the entry to nursing facility date, anticipated or actual discharge date, and community address with phone number, if known.
- Have the facility representative sign and date the form to confirm the accuracy and authorization of the information provided.
- Upon completion, the form should be sent to the dedicated fax number at (603) 271-7985. This ensures it reaches the Bureau of Elderly & Adult Services for processing.
Once the form is submitted, it triggers a review process by the Bureau of Elderly & Adult Services. They will assess the reported change and issue any necessary updates to the resident's status or care plan. For facilities and caregivers, understanding and executing this form with precision is paramount. It directly impacts the well-being and financial support of those in long-term care. Navigating this process with care and diligence ensures residents continue to receive the support they need without undue interruption.
Essential Queries on New Hampshire 3820
What is the New Hampshire 3820 form?
The New Hampshire 3820 form is a document used by the Bureau of Elderly & Adult Services to report a change of status, transfer, or discharge of a resident from a long-term care nursing facility. This form facilitates communication about Medicaid clients within the Integrated Care Facilities (ICF) and is essential for ensuring that Medicaid services follow the resident accurately and timely.
Who needs to fill out and submit this form?
The form is typically filled out by a representative of the nursing facility where the resident is located. It's their responsibility to report changes such as the beginning or end of a Medicare period, transfers between facilities, and discharges to the community, among other changes in the status of a Medicaid resident within New Hampshire.
How do you submit the 3820 form?
The completed form should be faxed to the Bureau of Elderly & Adult Services at (603) 271-7985. It’s important for the facility representative to ensure that all information is accurate and up to date before submission to prevent any delays in the resident's care or administrative confusion.
What information is required on the 3820 form?
You'll need to provide detailed information about the resident, including their name, Medicaid ID number, and the facility's contact info. Additionally, details about the specific status change such as Medicare start and stop dates, dates concerning transfers or discharges, and signatures from both the facility and BEAS representatives are necessary. This comprehensive data supports the effective management of a resident's care plan and Medicaid status.
When should the 3820 form be used?
It should be used whenever there's a need to notify the Bureau of Elderly & Adult Services about any change in the Medicaid status of a resident in a long-term care facility. This includes when a resident's Medicare coverage starts or stops, when they're transferred from one facility to another, or when they are discharged, either back to the community or due to passing away.
What happens after you submit the form?
After submitting the form, the Bureau of Elderly & Adult Services will process the information and make any necessary updates to the resident's Medicaid status. If the form reports a transfer, a new Notice of Medical Eligibility will be sent to the new facility. Submitting the form promptly helps ensure continuous Medicaid coverage and proper care coordination for the resident.
Is there a deadline for submitting the 3820 form?
While there's no specific deadline mentioned, it's crucial to submit the form as soon as possible after the change occurs. Prompt submission helps prevent any potential interruption in the resident's Medicaid coverage or care coordination.
Can the form be submitted for a resident not on Medicaid?
No, the 3820 form is specifically designed for reporting changes in the status of current Medicaid clients residing in long-term care nursing facilities. If the resident is not on Medicaid, this form would not be applicable for their situation.
Common mistakes
Filling out the New Hampshire 3820 form, essential for informing changes in status for long-term care nursing facility residents, requires attention to detail. Unfortunately, mistakes can happen. These errors can delay updates to a resident's care status, affecting both service provision and billing. Here are common mistakes to avoid:
- Not including the Medicaid ID Number can lead to significant processing delays. This number is critical for identifying the resident within the system.
- Forgetting to fill in the date of transfer when a resident is moved from one facility to another. This date is crucial for maintaining continuous care and billing accuracy.
- Omitting the Medicare start and stop dates for residents who transition from Medicare to Medicaid or vice versa. These dates ensure that billing is correctly aligned with the resident's coverage.
- Inaccuracies in the “Date of Death” section can cause unnecessary distress and confusion, requiring corrections that could have been avoided.
- Entering incorrect facility phone or fax numbers can impede communication between current and receiving facilities, especially for urgent matters.
- Failing to sign the form either by the facility representative or the BEAS representative. Unsigned forms are considered incomplete and will not be processed.
- Input errors in the “Change of date request” section, including the original approved start dates and the actuals, can cause billing and eligibility issues.
- Leaving the anticipated or actual date of discharge to community blank. This field is necessary for planning the resident's transition back to the community effectively.
- Mixing up the “Name of nursing facility being transferred to” and the “Name of facility being transferred from”. Such mistakes can create confusion and result in the resident's documentation being sent to the wrong place.
- Not updating or correcting information promptly when initial entries are found to be incorrect. Timely corrections ensure continuity of care and accurate billing.
Avoiding these mistakes ensures that the resident’s transition or status change is recorded accurately and promptly, facilitating seamless care coordination and financial transactions. Everyone involved in completing the form must double-check the details provided against the resident's records. In case of uncertainty, it’s better to verify the information with the proper authorities or departments before submission. Attention to detail can prevent a multitude of issues down the line.
Documents used along the form
When dealing with the New Hampshire 3820 form, which is vital for the Bureau of Elderly & Adult Services, specifically for managing long-term care nursing facility changes such as status updates, transfers, or discharges, it's essential to have all the documents that might be needed through the process. This form plays a crucial role in ensuring that transitions for ICF Medicaid clients between facilities or back into the community are smoothly facilitated. Alongside this form, there are several other documents that are often required to ensure comprehensive handling of a resident’s care and legal needs.
- Application for Medicaid: This document is needed to establish or validate the Medicaid eligibility of the resident involved.
- Advanced Directive Forms: These include living wills or durable power of attorney for healthcare, allowing the resident to outline their wishes concerning medical treatment and appoint someone to make decisions on their behalf if they're unable to do so.
- Asset Verification Form: This form helps in documenting the resident's financial resources, which is crucial for Medicaid eligibility determinations.
- Income Verification Form: Similar to asset verification, this document provides evidence of the resident's income sources.
- Physician’s Orders for Life-Sustaining Treatment (POLST) Form: It conveys the resident’s wishes regarding treatments they want or don't want at the end of their life.
- Resident Assessment Form: Used to evaluate a resident's condition and needs to ensure appropriate care is provided within the facility.
- Inter-Facility Transfer Form: Utilized when a resident is being transferred from one care facility to another, detailing medical information and the reason for transfer.
- Discharge Planning Checklist: This checklist ensures all necessary steps are taken and arrangements are made for the resident’s discharge back into the community or another care setting.
- Personal Inventory Form: A document to list personal belongings of the resident upon admission to or discharge from a facility, ensuring their possessions are documented and handled properly.
- Family Information/Contact Form: Records the contact information of family members or legal representatives to be notified about any significant changes in the resident’s condition or care plans.
Together, these forms and documents support the comprehensive management and coordination of care for residents transitioning between nursing facilities or from a facility back to community living. Ensuring that each of these documents is accurately completed and filed where necessary helps in the seamless provision of care and adherence to legal and procedural requirements. Understanding each document's role and how it complements the New Hampshire 3820 form can dramatically streamline the administrative and care coordination processes for elderly and adult services professionals.
Similar forms
The New Hampshire 3820 form is similar to other documents used in the healthcare and social services sectors, such as the MDS (Minimum Data Set) for nursing home resident assessment and the HCBS (Home and Community-Based Services) waiver service agreement forms. What makes these documents parallels is their role in facilitating transitions, whether for changes in service levels or transfers between care settings.
The MDS (Minimum Data Set) is a comprehensive assessment tool utilized across the United States in Medicare and Medicaid-certified nursing facilities. Like the New Hampshire 3820 form, the MDS is designed to collect critical information about a resident’s health, preferences, and needs to ensure they receive personalized and effective care. Both documents are crucial for coordinating appropriate levels of support and services for individuals in long-term care settings. The similarity lies in their detailed collection of resident information, which guides the care planning and monitoring process, although the MDS is more extensive and focused on assessment while the 3820 form targets status changes.
HCBS (Home and Community-Based Services) waiver service agreement forms are utilized to outline the specific services received by individuals under Medicaid waivers that allow for care in home or community settings instead of institutional care. These agreements share a common purpose with the New Hampshire 3820 form by documenting changes in service arrangements or provider information. Both ensure continuity of care through accurate record-keeping and communication between involved parties. While HCBS waivers typically emphasize maintaining individuals in their preferred living environment, the 3820 form focuses more on transitions for those already in or moving between institutional care settings.
Dos and Don'ts
Filling out the New Hampshire 3820 form, crucial for nursing facility status changes, transfers, or discharges, requires careful attention to detail. Here’s a guide on what to do and what to avoid for a smooth submission.
Do's:- Double-check all personal information: Ensure the resident’s name, Medicaid ID number, and the facility's contact information are correctly entered. Accurate data is crucial for processing.
- Specify the type of status change: Clearly indicate whether it’s a transfer, discharge, or change in Medicaid/Medicare status. This helps in maintaining accurate records.
- Include exact dates: Whether it’s for Medicare start and stop dates, date of transfer, or anticipated discharge to the community, precise dates are essential.
- Communicate with receiving facilities: If transferring, make sure you have the receiving facility’s correct name and contact information, and confirm they have space and resources to accept the transfer.
- Report changes timely: Submit the form as soon as possible to avoid delays in the resident's care or billing issues.
- Leave sections incomplete: Failing to fill out all sections relevant to the patient’s situation can lead to processing delays or errors in records.
- Use unclear handwriting: If completing the form by hand, write legibly. Unclear handwriting can lead to misinterpretation of vital information.
Accurate and timely submission of the New Hampshire 3820 form ensures uninterrupted care for residents and helps facilities maintain compliance with state regulations.
Misconceptions
Understanding the New Hampshire 3820 form can sometimes be challenging, leading to misconceptions regarding its purpose and use. Here, we aim to clarify some of these misunderstandings to ensure that the process involving long-term care nursing facility changes of status, transfers, and discharges are accurately managed.
It's only for internal use: A common misconception is that the New Hampshire 3820 form is intended for internal use within facilities. However, this form is crucial for communication between facilities and the Bureau of Elderly & Adult Services, ensuring that the necessary state departments are informed of any changes in a resident's status.
It's applicable for all patients: This form is specifically designed for current Intermediate Care Facilities (ICF) Medicaid clients. It's not applicable to patients in other types of care or those not on Medicaid, which is a detail sometimes overlooked.
It's only about discharge notices: While the form includes fields for discharge information, its scope is broader, covering changes of status, transfer between facilities, and even death notifications, making it an important document for a range of situations.
No need to inform Medicaid separately: There's a belief that filling out this form negates the need to inform Medicaid of any changes. However, this document serves as a notification to involved parties including Medicaid, and ensuring all parties have updated information is crucial for continued coverage and compliance.
Medicare details are not necessary: Since the form is used for Medicaid clients, the inclusion of Medicare start and stop dates might confuse some. These details are vital for patients who are transitioning between Medicare and Medicaid or have dual eligibility, offering a complete picture of their coverage status.
Any staff member can sign it: The form requires signatures from both facility and BEAS representatives. This ensures that the information is verified and officially acknowledged by both parties, so not just any staff member's signature is appropriate or sufficient.
It's only for nursing facilities: Though primarily used by nursing facilities, the form is also applicable to transfers from a Chronic Care Facility (CFI) to a nursing facility, expanding its applicability beyond nursing homes alone.
It's a onetime form: Another misunderstanding is that this form is filled out once and then no longer needed. In reality, any time there is a change in a resident's status, including transfers, discharges, or death, a new form must be filled out and sent, ensuring ongoing communication and compliance with state requirements.
Clarifying these misconceptions is crucial for the proper use of the New Hampshire 3820 form. By understanding its purpose, requirements, and application, facilities can ensure that they are in compliance with regulations and providing the necessary care and information for their residents.
Key takeaways
Filling out and using the New Hampshire 3820 form is a crucial process for managing the care transitions of residents in long-term care settings. This form serves as a formal notification mechanism for various status changes, including transfers and discharges. Understanding its components and requirements can ensure these transitions are handled efficiently and in compliance with state regulations. Here are five key takeaways to consider:
- Specifically Designed for Current ICF Medicaid Clients: The New Hampshire 3820 form is tailored for individuals who are already under the Medicaid program in an Intermediate Care Facility (ICF). It's used to notify changes related to their Medicaid status, such as Medicare start and stop dates, and transitions between facilities.
- Comprehensive Change Notification: The form captures a wide range of status changes, including transfers between nursing facilities, changes in Medicaid eligibility dates, discharge details, and even the resident's death. This ensures all relevant parties are aware of the individual's current situation and care requirements.
- Facilitates Smooth Transitions: By providing details of the facility a resident is being transferred from and to, including contact information and transfer dates, the form plays a pivotal role in ensuring a smooth transition from one care setting to another. This is vital for the continuous care and wellbeing of the resident.
- Information on Discharge to Community: For residents transitioning from a nursing facility back to the community under the Community First Initiatives (CFI) program, the form includes sections to detail anticipated or actual discharge dates, along with the community address. This helps in planning and facilitating community reintegration.
- Requirement for Signatures: The completion and authenticity of the form require the signatures of both the facility representative responsible for the resident's care and a representative from the Bureau of Elderly & Adult Services (BEAS). This dual signature requirement underscores the form's importance in the official documentation and communication process regarding long-term care residents' status changes.
Properly understanding and utilizing the New Hampshire 3820 form is essential for healthcare providers in the state. It not only ensures compliance with regulatory requirements but also supports quality care coordination and management for elderly and adult residents in long-term care settings.
Different PDF Templates
Nh Self Employment Tax - The form’s comprehensive nature requires thorough documentation and verification of compensation payments, encouraging meticulous record-keeping.
New Hampshire 2620 - Changes in provider information such as address, incorporation status, or name must be reported using a new New Hampshire 2620 form alongside an alternate W-9 form.